According to the statistics and recent studies by government organizations, Dentistry related professions, including dentists, dental hygienists, and dental technicians rank amongst the top 4 of the most dangerous professions surveyed. That list included chemical factory-related professions and metal pourers.
But what makes the dentistry profession so dangerous?
What are the Risks?
Dentists and dental hygienists are routinely exposed to many forms of airborne contaminants.

They come from dental procedures including root canals, implants, extractions, and scaling.
These procedures are called aerosol-generating procedures (AGPs).
They form saliva-laden splatter rich in blood, plaque, debris, secretions from the gums and the micro bio-flora from the oral biofilm which is home to over 1000 different species of micro-organisms. Some of the most worrisome sources of airborne contamination in dentistry are bioaerosols, mixtures of air from a handpiece, water from the dental-unit waterline, and debris from the patient’s mouth.
Many of the micro-organisms can be infectious, and they can also get aerosolized into particulate sizes less than 0.1 to 4 um. These microscopic droplets can hover in the air for up to 6 hours and have a substantial range.
The larger saliva-laden splatter naturally deposits on all surrounding surfaces like the floor, chairs, surfaces, masks, equipment, face, mouth, eyes and skin, hands and clothing of the provider and patient.
However, the bioaerosols can get suspended in the air, and find their way around the dentistry through the HVAC system and through air movement between spaces.
A “Toxic Cloud” of Bio-Aerosols
As one American dentist described it, “a toxic cloud spans from the floor to a height of six feet. The concentration of bacteria in this cloud is usually as high as 100,000 bacterium/cubic feet of air. Among the pathogens commonly found in this “cloud”:
- Staphylococcus aureus
- Acinetobacter wolffii
- Legionella
- Aspergillus
- Mycobacterium tuberculosis
- Streptococcus
- Varicella-zoster
Bio-aerosol concentrations in the dental setting skyrocket during and immediately after dental treatments.
Can they transmit between spaces and people? – Most definitely!
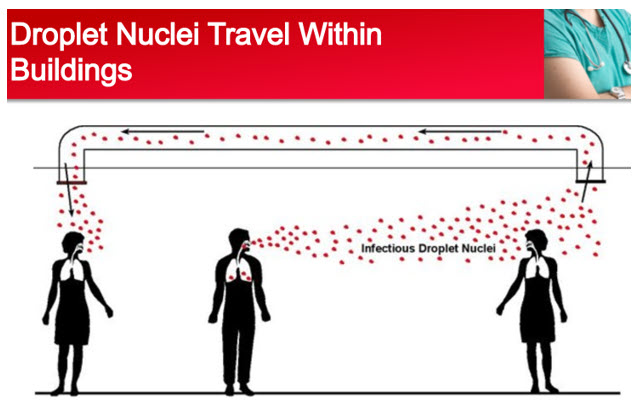
Aerosolized pathogens have extremely significant travel ranges from 160 to 200 ft. These airborne pathogens / commensals can stay in the air for long periods of time and travel through the building’s HVAC system.
Closing the Loop in Infection Control
In healthcare, air quality is one of the most easily forgotten components that have a significant impact on the health of indoor occupants.
The constant traffic of patients, staff and visitors, the use of high-speed mechanical tools (Aerosol generating procedures) are all generators and contributors to aggregate microbial contamination.
Another aspect often overlooked, is the use of chemicals in cleaning and sterilization of dental clinics. These chemicals can release volatile organic compounds into the air or VOCs which can affect the health of the space occupants.
Dental protocols are usually comprehensive to address contamination from hands/skin and surfaces but are not enough to mitigate the microbial burden from air contamination.
Air disinfection thus becomes one of the most critical and overlooked factors in the design of dental clinics which could have an impact on the safety and wellbeing of patients, staff, and visitors alike.
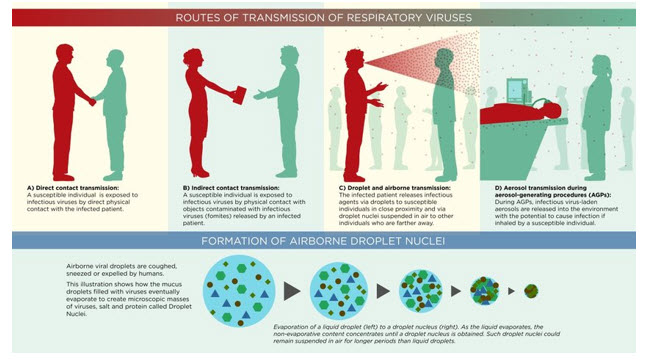
The others are surfaces and hands/skin. Reiterating the three important factors that need to be looked at for effective infection control, they are
- Hands/Skin (Direct Contact Transmission)
- Surfaces (Indirect Contact Transmission)
- Air (Airborne Transmission)
- Aerosol Transmission (during and after Aerosol Generating Procedures)
So, how can we mitigate these risks?
The risk for infection can never be completely eradicated but the probability of infection and transmission can be reduced substantially. The 4 steps of risk mitigation include an acceptance of the risk, avoiding the risk, reducing the risk, and transferring the risk
By means of:
- Architectural Design of Spaces to minimize transmissibility of aerosols and negative pressurization of spaces is the first step in the process. – Acceptance of Risk. The layout should always be optimized to mitigate risks present. This affirms an understanding and acceptance of the risk and sets the stages to a successful dental setting.
- Engineering Controls including ventilation, pressurization, filtration, source capture hoods, filtration units with HEPA filtration units and Germicidal UVC and activated carbon media for mercury mitigation, centralized systems capable of air filtration. Engineering controls are the second step and should be designed to completely avoid the indoor risks to occupants and environmental risks present to the public.
- Personal Protective Equipment including high volume evacuators, saliva ejectors, face shields, extra oral suction devices with hoods encapsulating patients, masks (N95), surgical masks (not very effective). – This should be considered only as a last resort if adequately designed systems are not present to protect space occupants. This reduces risk but is not a fail-safe method of mitigation.
- Administrative & Procedural Controls – usage of spaces based on their design, fallow times between patients in a space based on ventilation rates, scheduling strategies for Aerosol generating procedures (AGPs) in rooms and minimization of AGP procedures, surface disinfection protocols etcetera.- Risks are not mitigated in this case but only transferred from one occupant to another. It is like an insurance policy in the sense that one party is always exposed to the risk. Risk reduction strategies need to be used in conjunction with such controls to protect indoor occupants.

“Every patient should be treated as potentially infectious.”
Dental procedures on patients need to be conducted under protected environments to ensure the safety healthy of your staff, including hygienists, and dentists.
In today’s pandemic world, no precaution can be deemed excessive.
High volume evacuators, preprocedural rinse, face shields are recommended by the Alberta Dental Association and College, all of which are steps in the right direction towards mitigating these risks.
We should be cognizant of the fact that
“There is no threshold for concentration of viruses, pathogens and particulates in causing infectious disease”
An evacuator that reduces the concentration of contaminants from 5 mg/m3 to 0.5 mg/m3 is still of no use as the number of viruses in the lowered concentration could be still be equally infectious as the unmitigated volume.
And as they say,
NEVER GUESS ABOUT AIR FLOW. AIR HAS A MIND OF ITS OWN.
Lexus Engineering will help you visualize your airflow and help you optimize it through advanced CFD software.
WHAT IS CFD? How can it help us?
A CFD (Computational Fluid Dynamics) study can be used to understand airflow dynamics in any space and airflow patterns can be optimized based on this study by the correct placement of diffusers and grilles.
The picture below shows airflow patterns and the path of airborne contaminants based on a CFD Analysis.
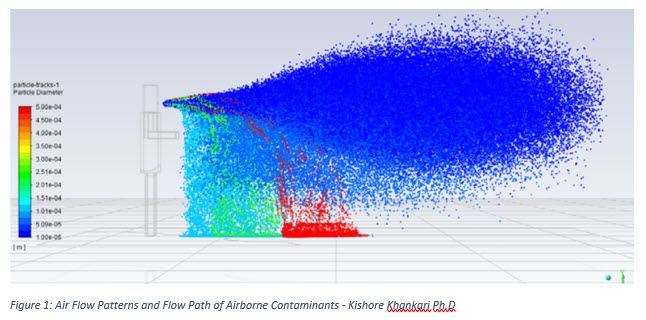
- Large particles/droplets fall near the source
- Small particles/aerosols remain airborne
- Aerosols follow the path of flow of air
- Density, shape, and size of particles will affect its dynamics
- Droplets can evaporate and become aerosol and airborne
- External forces like a fan (HEPA Unit) can affect the trajectory if the aerosols are on the positive pressure side of the blower
How can Lexus Engineering help you?
We at Lexus Engineering are specialists in the field of indoor air quality.
Our research and expertise will help guide you to make targeted choices for your clinical needs. We can assist you in picking the right solution to make your clinic a safer one.
Custom packages can be designed to best cater to your clinic’s requirements. Call us today for a free HVAC assessment at 780-435-4544 and find out how we can help you.
References:
1. Efficacy of High-volume Evacuator in Aerosol Reduction: Truth or Myth? A Clinical and Microbiological Study
2. A laboratory comparison of evacuation devices on aerosol reduction
3. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications
4. Role of preprocedural rinse and high-volume evacuator in reducing bacterial contamination in bioaerosols
5. Dentistry, Technology and HV-Evolution
